Pharmacogenomics: Personalising medication to suit your DNA
Pharmacogenomics enables clinicians to personalise their patient’s medication and individualise drug selection and dosage. This ensures the patient gets the optimal level of care and experiences minimal drug interactions.
The human body can be compared to a computer. Your DNA is arranged into smaller parts called genes. These genes can be considered as the “code” that acts as the information system, influencing both the inward functions and outward appearance.
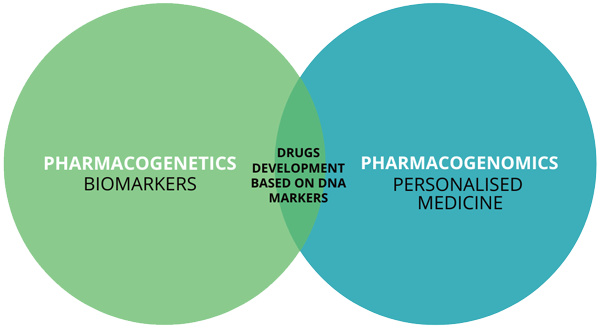
Both Pharmacogenetics and Pharmacogenomics have an impact on the methodologies behind genetic testing and personalised medication. Thus, helping to improve drug selection, dosing, drug efficacy and toxicity (Figure 1).
We’ve all been patients at some point of our lives. Some of us have had medication prescribed to us that either generated terrible side effects or was not effective at all. This is where pharmacogenomics comes in. Instead of using the “one-dose-fits-all” approach, clinicians are able to personalise medication for each individual patient. The way to achieve this is through genetic testing.
Integrative health solutions are patient-centric, meaning the more personalised the treatment is, the more our patient’s needs are being met. Using pharmacogenomics (genomic insight testing) aids the patient in being able to gain a certain amount of autonomy over their health status.
Pharmacogenetics vs. Pharmacogenomics
Pharmacogenetics is the study surrounding the genetic differences in single genes and how they influence a person’s ability to metabolise a drug. Whereas pharmacogenomics studies whole genome differences in multiple genes and multiple SNPs and how they influence variability in the drug response. It is that which aids clinicians in their ability to personalise their patient’s medication. Specialists use this information to individualise drug selection and drug dosage. This is to avoid drug reactions, and to maximise drug efficacy.
Medication and metabolism
When drugs enter the body, they are metabolised and altered by enzymes. These enzymes either activate or deactivate the drug administered. The most well-known of these enzymes is Cytochrome P450 (CYP450). Figure 2 depicts the different types of isozymes of the CYP450 enzyme. There are over 50 of these isozymes, 7 of which are involved in metabolising over 80% of medication.
One would perhaps ask why this is important? Simply put, it is important in determining the level at which a person metabolises a certain drug. There are three categories of metabolisers, which all depend on the combination of CYP2D6 alleles.
Metabolisers, Inducers and Inhibitors
An important aspect when looking at genomic results is referring to metabolisers, inducers and inhibitors. An inducing agent is a drug that increases the rate of another drug’s metabolism by inducing P450 enzymes. They’re responsible for about 90% of drug metabolism.
By increasing the drug’s metabolism, it affects the drug’s reaction within the body. Inhibitors will block the metabolic activity of one or more of the P450 enzymes. The extent to which an inhibitor affects the metabolism of the drug depends upon the dose and the ability of the inhibitor to bind to the enzymes. This might lead to increased or unwanted drug reactions or side effects.
Knowledge of the patient’s genes allows you to look at the metaboliser type that the patient falls under, which SNP data can help identify and outline more effectively.
Types of metabolisers
Genetic testing can be used to predict how a person will metabolise or react to a particular drug. Currently, there are three main types of metabolisers a person can be classified under, this being a poor metaboliser, intermediate metaboliser and ultra-rapid metaboliser. It is important to understand this when dealing with your patient’s drug selection, as certain drugs may have more positive or negative outcomes. Hence, where pharmacogenomics comes in.
Poor metabolisers experience a very slow breakdown of medication, making the side effects more pronounced. This may indicate that the standard dose of certain medication may not work as intended.
Intermediate metabolisers break down medication slowly with minimal side effects although overdosing is still possible.
Ultra-rapid metabolisers break down medication too quickly, which means that dose of the drug may not be enough, so the patient may not get relief from the symptoms.
Summary
Pharmacogenomics enables a clinician to personalise their patient’s medication and to individualise drug selection and dosage, lowering the chances of overdosing and experiencing side effects. Pharmacogenomics takes into account an individual’s rate of metabolism, ensuring the correct dosage is prescribed, providing the patient with the optimal level of care. Remember, it is also important to look at the medication your patient is currently on to minimise interactions as some medications/supplements can cause a drug to react differently to what it would under normal circumstances.
How do I Become a Functional Medicine Practitioner to learn more about Pharmacogenomics?

The Institute of Integrative Medicine is a global leader in the field of Integrative Medicine Education. Integrative medicine aims to be at the forefront of modern technology and new discoveries. We offer certified online courses helping you to take charge of your practice and improve the quality of life for your patients. Find out more about the courses we offer today!
More posts in this category:
An Integrative Approach to Amino Acids
Amino acids are integral in several bodily functions. They are the building blocks of proteins that aid in multiple functions on a cellular level. We cannot forget about crucial amino acids, as they aid in immune function, muscle growth and recovery, and can be utilised in treating deficient hospitalised patients. Amino acid testing and supplementation can improve lifestyle and wellbeing.

How Amino Acids can improve your Exercise Regime
Branched-chain amino acids are extremely valuable for exercise, muscle preservation and growth. Not only can they reduce muscle loss and damage, they can also help grow and repair muscle. Consuming BCAAs can improve strength, endurance and reduce fatigue during exercise.

Amino Acid Deficiencies and Symptoms
Blood tests are one of the most common and best ways to identify amino acid deficiencies. Amino acids are vital in the optimal functioning of the body and can lead to uncomfortable symptoms when not monitored regularly. The development of mood disorders, experiencing a lack of focus and fatigue, and a weak immune system may be signs of an amino acid deficiency. The appropriate treatment of these deficiencies are essential to improve overall health.
